In this interview, News-Medical speaks to Professor Kevin Baird about his lifelong research into malaria and how another malaria parasite, P. vivax, is taking a toll on global health.
Please could introduce yourself, tell us about your background into neglected tropical diseases (NTDs), and what inspired your latest research into malaria?
I have been involved in research on malaria as a scientific, clinical, and public health problem for the past 40 years. For 22 of those years, I was a malaria specialist on active duty in the US Navy Medical Service Corps, serving at varied duty posts around the world. Early in that journey, I began research on Plasmodium vivax. At that time, almost no one was doing work on this parasite because it was broadly accepted as causing an essentially benign infection.
The inspiration for the work with Katherine Battle (a former student at Oxford and now colleague) comes from a decade of work trying to understand how to measure the incidence and burden of P. vivax globally.
Our review paper articulates a long-held concern regarding the reliability of patent parasitemia as the basis of measuring the global burden of this infection. Recent findings by many others regarding tropisms of P. vivax for tissues beyond the vascular sinuses gave us the confidence to express those concerns.

Image Credit: nechaevkon/Shutterstock.com
Malaria is recognized as a serious tropical disease with much research focusing on the most common malaria parasite (Plasmodium falciparum). Why is it still just as important to look at the health effects of other malaria parasites including Plasmodium vivax?
Yes, all of the malaria parasites – there are five of them that naturally infect us – cause serious illness. Some do so less frequently than others, and sometimes differently even within the same species. An abundance of evidence gathered over the past 15 years leaves almost no doubt that the “benign tertian malaria” caused by acute P. vivax malaria will often result in severe and life-threatening syndromes without prompt diagnosis and effective treatment. The notion of so-called benign and malignant species of malaria parasites is dangerous dogma to patients suffering P. vivax malaria.
We are also beginning to learn a great deal more about the harm done by chronic infection of low or moderate febrile illness, and by repeated attacks of acute malaria over years. The idea that the harm of malaria is done solely by the acute attack with patent parasitemia is a global Northern bias, and that finds expression in how the global burden of P. vivax is estimated, that is, by estimating those attacks.
In your latest review, you look at P. vivax and its effect on global health. How did you carry out this review and what did you discover?
We simply examined the emerging understanding of the biology of P. vivax in humans – with its profound tropisms for tissues beyond peripheral blood – and logically considered how those may impact current global burden estimates.
You described that statistics may often miss the harm done by P. vivax which often affects impoverished communities. Why is this and why do you believe it is likely that these attacks are missed?
Consider the statistic – acute febrile illness in a patient diagnosed with malaria, usually by microscopic or immunochromatographic examination of peripheral blood. First, we know P. vivax occurs at lower levels of parasitemia compared to P. falciparum and will therefore more often be missed even if the harmful biomass in the patients is equal.
Patients having fevers of unknown origin dominate the wards of many hospitals in impoverished areas – absent a definitive diagnosis they are often treated presumptively with antibiotics or antimalarials. If P. vivax is not seen, it is of course uncounted. When we say “obscure”, this is what we mean.
Then there is the harm done with chronic P. vivax malaria of periodic or mild symptoms that does not rise to a visit to a hospital or clinic. The patients may endure weeks or months of deepening anemia, emaciation, weakness, and, in small children, significant cognitive impairment.
The chronic infection is most often not detectable by conventional diagnostics, and the harm done is slow and incremental. It is also uncounted in global burden estimates. When we say “insidious”, this is what we mean.
Image Credit: Novikov Aleksey/Shutterstock.com
A groundbreaking milestone has also just been reached regarding malaria and the roll-out of the RTS, S/AS01 vaccine in Africa. What effect do you think this will have on malaria cases and do you believe we will then see a rise in P. vivax infections?
That vaccine, presuming it delivers the benefits hoped for, will mitigate serious illness and mortality caused by P. falciparum among small children in Sub-Saharan Africa. It does not, however, appear to offer a sterilizing immunity from that infection.
People are still infected and parasitemic, but less often seriously ill. Falciparum malaria infections may not decline, but the harm done will hopefully be less frequent. In that perspective, no, I do not see P. vivax becoming somehow more prominent.
In any event, P. vivax in Sub-Saharan Africa is complicated by the dominance of people who do not express a molecule on their red blood cells called the Duffy factor. We have long accepted P. vivax required that molecule to invade red blood cells and this explained the broad absence of endemic P. vivax in much of Sub-Saharan Africa.
Recent work, however, demonstrates alternative invasion pathways and the raw fact of Duffy-negative Africans having viable P. vivax within red blood cells. We may now well wonder if the paucity of endemic P. vivax in this region is an illusion.
How will treatment approaches and diagnostics need to differ for P. vivax compared to P. falciparum?
The hepatic latency of P. vivax, which does not occur in P. falciparum, imposes a very complex and difficult therapeutic problem. It requires a different class of drugs, the 8-aminoquinolines, and those are dangerously toxic in patients having an inherited defect of glucose-6-phosphate dehydrogenase deficiency – which occurs in about 8% of populations of nations having endemic malaria transmission. We have no other class of drugs for this treatment, and it is a very serious problem.
But it is the diagnostics for P. vivax that very probably need to significantly depart from what works for P. falciparum. If we accept the emerging understanding of P. vivax biology in the human host as having profound tropisms for tissues beyond peripheral blood, then we must accept the frank inadequacy of the examination of that compartment as a means to determine the presence or absence of P. vivax.
I am involved with serological diagnostics which are quite promising and exciting. We may see validation of serological signal as evidence of the presence or absence of P. vivax in any human tissue.
How will your review help researchers to further understand the biology of P. vivax and its effects on global health?
Simply put, we hope the review will alert researchers to the inadequacy of conventional diagnostics as a clinical and public health instrument in the case of P. vivax malaria. That allows us to view estimates of burdens with appropriate skepticism, and to aspire to develop the technologies that will ultimately reveal the true burdens of infection, illness, and death caused by P. vivax malaria.
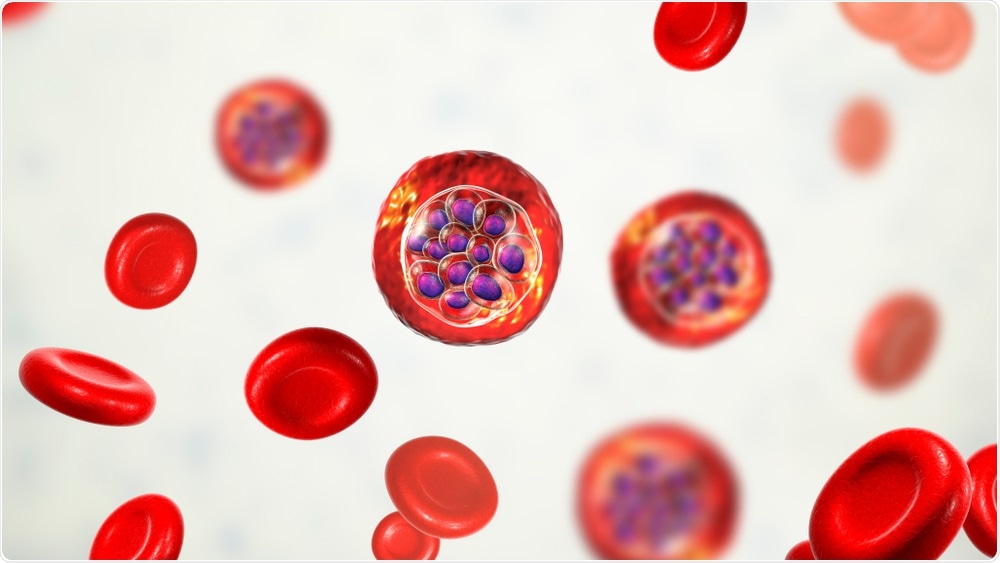
Image Credit: Kateryna Kon/Shutterstock.com
Do you believe that with continued funding into malaria research, we one day will see a world without malaria?
Yes, I am very confident we will “one day” see a world without malaria as a tragically huge cause of illness and death. I also earnestly believe that research, properly supported, will shorten the span of time we wait for that day. There is so much we don’t yet understand, and no one should underestimate the ability of these parasites – so highly evolved and complex – to frustrate our human ambitions.
Our current tools are too crude and blunt to see a malaria-free world any time soon. Research and better tools and understanding will, eventually, get us there.
What are the next steps for you and your research into malaria?
I am keen to conduct meaningful serological surveys of large populations to derive credible estimates of the prevalence and incidence of infection by P. vivax.
Where can readers find more information?
This recent review offers a deeper exploration of breaking P. vivax biology and its practical implications.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8447957/pdf/fcimb-11-696598.pdf
About Professor Kevin Baird
I am the founding Director of the Eijkman-Oxford Clinical Research Unit within the Eijkman Institute of Molecular Biology at Jakarta, Indonesia, established in 2008.
I am a Professor of Malariology in the Centre for Tropical Medicine and Global Health, Nuffield Department of Medicine, University of Oxford, United Kingdom.









 Add Category
Add Category

.png)