In this interview, News-Medical talks to Dr. Brendan Horton about his latest research which has shed new light on cancer and T cells, and how this knowledge could be used to develop more effective and innovative cancer therapies.
Please introduce yourself and tell us about what led you to research T cells and cancer therapy.
I am a post-doctoral researcher in Dr. Stefani Spranger’s laboratory in the Koch Institute for Integrative Cancer Research at the Massachusetts Institute of Technology. Before I started at MIT, I received my Ph.D. at the University of Chicago where I studied the functions of T cells that infiltrate tumors.
I had always been fascinated by the immune system’s potential to be harnessed for anti-cancer therapy, and the clinical success of immune checkpoint blockade drove me to continue studying how T cells responding to tumors behave when immunotherapy is successful or not.
What is non-small cell lung cancer (NSCLC)?
Non-small cell lung cancer (NSCLC) is a leading cause of cancer-related death both around the world and in the United States. Like many cancers, NSCLC is not one disease but a heterogeneous collection of multiple cancer subtypes. The most common subtype of NSCLC is adenocarcinoma, which is also the subtype of NSCLC that we modeled in our study.
Which treatment an NSCLC adenocarcinoma patient receives depends on what mutation drives their cancer. Patients whose cancers are driven by mutations in genes EGFR or ALK generally receive small molecule inhibitors that target the corresponding mutated proteins, while patients with KRAS mutations may be eligible to receive immune checkpoint blockade (ICB).
However, many patients who receive ICB still do not respond to this therapy, and understanding mechanisms of ICB resistance is a major goal for the immune-oncology field.
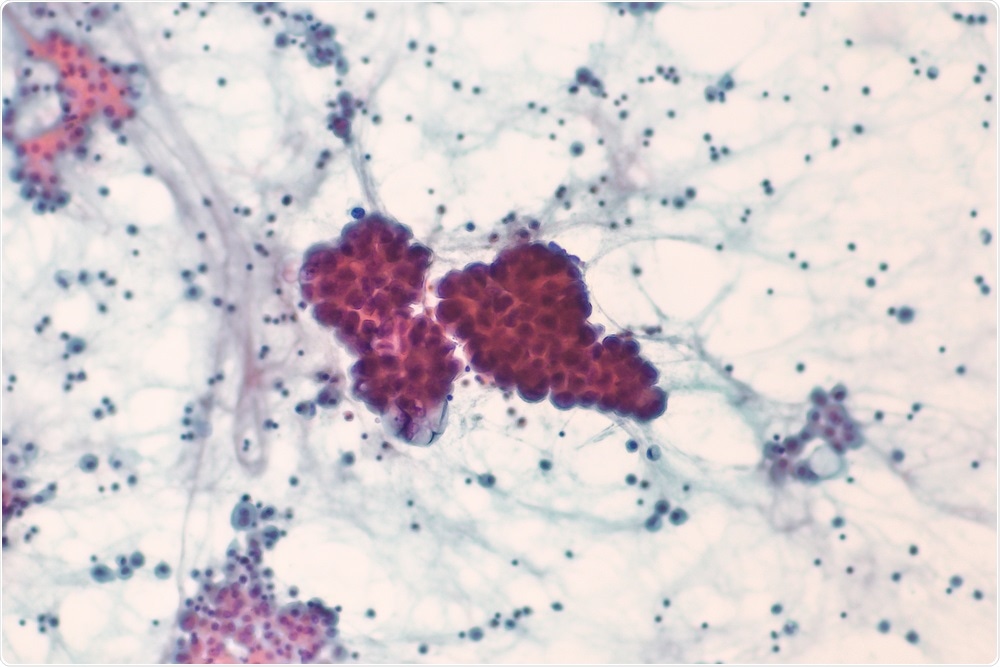
Image Credit: David A Litman/Shutterstock.com
How does immune checkpoint blockade (ICB) therapy work and what are its limitations?
The immune system is comprised of many cell types, and T cells are one critical type of cell that protect the body from certain types of immune challenges, including viral infections and cancer. When T cells become activated during an immune response, they express receptors on their cell surface called checkpoints. These checkpoint receptors dampen T cell function and are a normal part of the immune response that plays an important role in limiting damage to normal tissue and preventing autoimmunity.
However, tumors can upregulate ligands of checkpoint receptors to co-op their immune-dampening function and prevent T cells from killing tumors cells. ICB are antibodies that bind checkpoint receptors or their ligands, blocking their interaction and increasing anti-tumor T cell function. The main limitation of ICB is that it can only enhance an ongoing immune response, and it is thought that many patients that do not respond to ICB either have too weak of an immune response or have tumors that are able to prevent T cell entry into the tumor microenvironment.
What does your research show about possible explanations for T cells not responding to ICB? How does this challenge previous thinking?
As ICB enhances anti-tumor T cell function, the infiltration of activated T cells into tumors is usually a positive prognostic factor for a good response to ICB. Many times resistance to ICB is thought to occur due to a lack of anti-tumor immune response, or due to the tumor being able to exclude T cells. However, not every patient with a T cell-infiltrated tumor responds to ICB, and very little is known about how T cell-infiltrated tumors become ICB resistant.
In our model, we found that lung tumors were resistant to ICB not due to a lack of T cells, but because the anti-tumor T cells were unable to be reinvigorated by ICB. By profiling the gene expression of tumor-infiltrating T cells, we found that their gene expression patterns appeared distinct from tumor-infiltrating T cells that had been previously described.
Additionally, these gene expression patterns appeared to be established during T cell activation in the tumor-draining lymph node, before the T cells even entered the tumor. These two aspects, that activated, tumor-infiltrating, tumor-specific T cells can enter into a state that does not respond to ICB, and that this state is induced early during T cell activation before the T cells enter the tumor, are not currently well appreciated, and indicate that a subset of NSCLC patients may not respond to ICB because of how their anti-tumor T cells were activated.
How did you design your study to determine why some tumors are resistant to ICB?
Using a transplantable mouse lung cancer, we compared tumors growing in lungs with tumors growing subcutaneously, which is the most common method of growing tumors in mice. We found that lung tumors were resistant to ICB, but that subcutaneous flank tumors were sensitive to ICB. When we found that lung tumors were ICB-resistant despite being infiltrated by activated T cells, we realized we could use this system to compare the immune responses generated against lung and flank tumors to compare T cells in ICB resistant and sensitive tumors.
We collaborated with Dr. Chris Love’s laboratory to utilize their Seq-well platform to analyze T cell gene expression by single-cell RNA sequencing. This was a critical collaboration as the resulting gene expression profiling paved the way for understanding that lung tumor-infiltrating T cells were distinct from previous analyses of tumor-infiltrating T cells.
Using these gene expression signatures, we were able to determine that there are analogous T cells in human NSCLC patients, suggesting that this ICB-resistant T cell gene expression pattern might be responsible for ICB resistance in certain NSCLC patients. However, further clinical data will be required to definitively test that hypothesis.
Image Credit: StudioMolekuul/Shutterstock.com
What do your team propose to be the underlying cause of ICB resistance?
There are likely many different underlying causes of ICB resistance across different patients. However, our study suggests that in at least a subset of ICB-resistant tumors, ICB resistance stems from the conditions in which anti-tumor T cells were activated in tumor-draining lymph nodes. Overcoming this resistance will require being able to reprogram these T cells into a more functional state.
How did your team use cytokines to counteract ICB resistance and why is this currently not appropriate for use in humans? How could this change in the future?
By comparing gene expression profiles of T cells from ICB-resistant lung tumors and ICB-sensitive flank tumors, we found that T cells responding to lung tumors had lower expression of receptors for the cytokines IL-2 and IL-12, which are important cytokines for T cell activation and differentiation.
We collaborated with Dr. Dane Wittrup’s laboratory to test if delivering IL-2 and IL-12 to lung tumor-bearing mice could overcome lower cytokine receptor levels on T cells and lead to better lung tumor control. And indeed, we found that lung tumors were better controlled after combined administration of IL-2 and IL-12.
In humans, however, these cytokines are known to have high levels of toxicity that make them currently unsuitable as therapeutics. But many researchers are actively working on either engineering these cytokines to reduce their side effects, or on developing better delivery systems to target cytokines specifically to tumors to avoid toxicity. With improvements in cytokine engineering and delivery systems, we could better harness the anti-tumor power of these molecules while avoiding their high toxicity.
How could the knowledge gained from your research be used to treat non-small cell lung cancer more effectively with more innovative cancer therapies?
Biomarkers of ICB response are actively being sought to better predict which patients will benefit from ICB. If we can utilize tumor-infiltrating gene expression profiles to predict which patients will respond to ICB and which won’t, patients could be better matched to the treatments that would provide them with the most benefit.
Combined with safer approaches for cytokine therapy, gene expression profiling of tumor-infiltrating T cells could determine which patients would respond to ICB, and which would need other approaches, such as cytokine therapy, to reinvigorate their anti-tumor T cell response. Additionally, realizing that the conditions during T cell priming are critical for later anti-tumor T cell function could help researchers optimize vaccination strategies, where the goal is to prime new anti-tumor T cells to induce tumor control.

Image Credit: didesign021/Shutterstock.com
What is the next step for this research?
We are very interested in determining more about the molecular programming in T cells that drives them to become ICB resistant. The more we can learn about how ICB resistance is established, the more potential strategies we can come up with for overcoming this resistance and improving cancer immunotherapy.
What does the future of cancer therapy look like to you?
I imagine a type of personalized cancer therapy where our ability to quickly profile tumor mutations and immune cell differentiation states result in patients being paired with the optimal treatment options for their individual tumor status, whether it be chemotherapy, small molecule inhibition, checkpoint blockade immunotherapy, adoptive cell therapy, cytokine therapy, or vaccination against tumor neoantigens.
Likely, effective cancer therapy will involve developing optimal combinations of these therapeutic strategies to minimize the development of treatment resistance and enable long-term anti-tumor responses.
Where can readers find more information?
About Dr. Brendan Horton
As a post-doctoral researcher, I carry out independent research while receiving scientific and career mentorship from the laboratory principal investigator, Dr. Stefani Spranger. Publishing this work in Science Immunology has absolutely been a career highlight.
I have been able to present this story at this year’s Immune Oncology Young Investigator Forum and the Cytokines in Cancer Immunotherapy Workshop, and will present in November at the Society for Immunotherapy of Cancer Sparkathon Accelerator, and have received a travel award to share this work at the Society for Immunotherapy of Cancer annual meeting.








 Add Category
Add Category

.png)