Although monkeypox virus infection was predominantly found in West and Central Africa, since May 2022, this double-stranded DNA virus has been reported in many countries outside Africa. Similar to the smallpox virus, the monkeypox virus also belongs to the orthopoxvirus family and is less severe. The World Health Organization recently declared the global monkeypox outbreak a public health emergency of international concern.
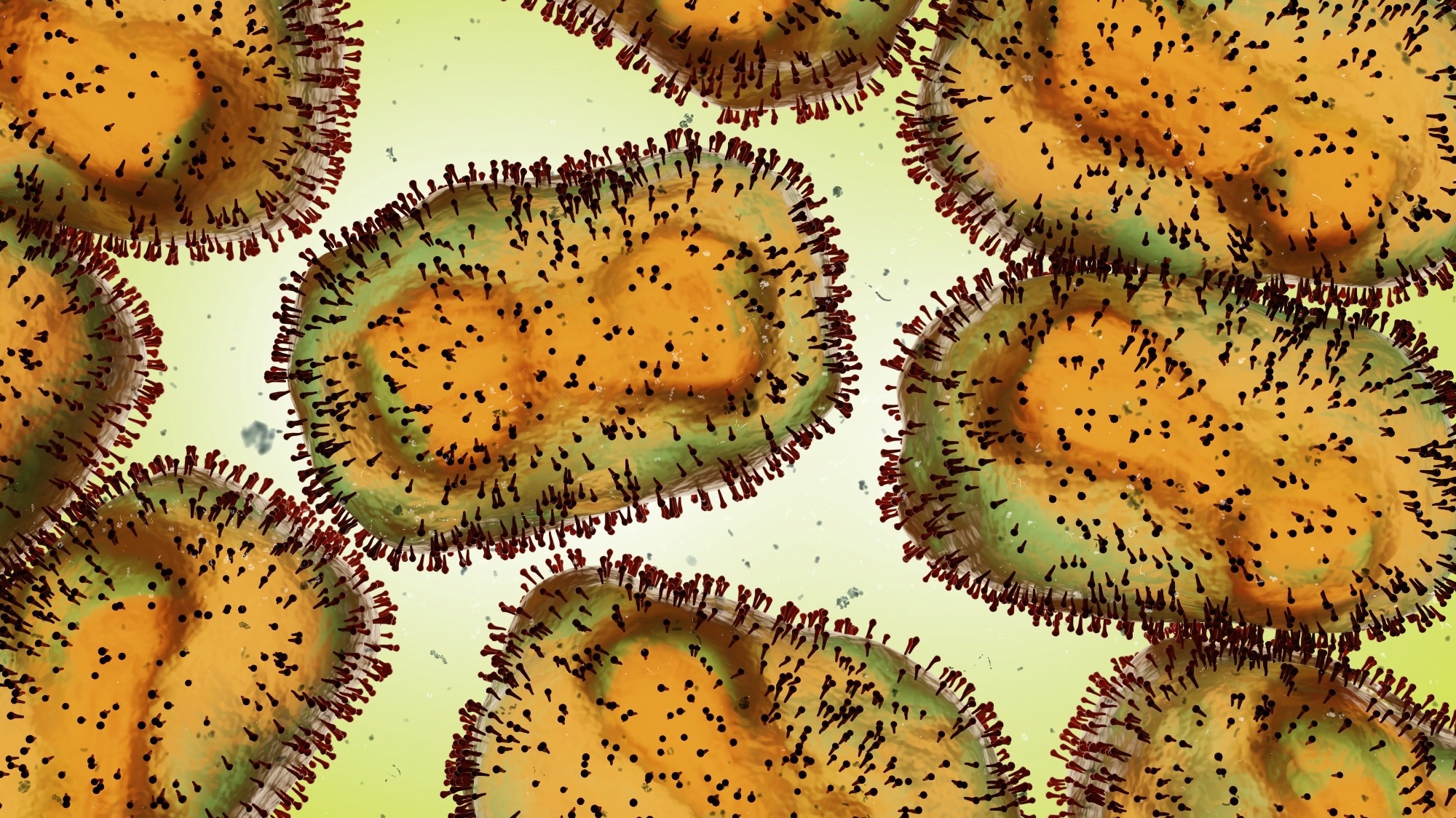 Study: A bioinformatics approach to systematically analyze the molecular patterns of monkeypox virus-host cell interactions. Image Credit: Dotted Yeti / Shutterstock
Study: A bioinformatics approach to systematically analyze the molecular patterns of monkeypox virus-host cell interactions. Image Credit: Dotted Yeti / Shutterstock
Background
Typically, monkeypox disease symptoms last around 2-4 weeks, with a low mortality rate of 3.6% in West Africa and 10.6% in the Congo Basin. The incubation period of this virus is between 5 and 21 days, which is not infectious. Monkeypox-infected patients experience headaches, fatigue, fever, muscle soreness, and lymphadenopathy. Within three days of infection, rashes appear on different body parts, such as the face, hands, legs, oral mucosa, conjunctive, genitals, and cornea.
Two main routes for disease transmission are animal-to-human transmission and human-to-human transmission. Recent monkeypox outbreak-related studies have reported transmission through MSM (men who have sex with men).
The majority of available data based on monkeypox disease infection are case reports. Very few studies are available on the interactions between the virus and the host. It is essential to understand the underlying mechanisms associated with monkeypox interactions with humans to cause severe infection. This information could help develop effective treatments to cure and prevent monkeypox infection.
A recent study posted to the bioRxiv* preprint server reported the interaction between monkeypox and human cells. Molecular sequences were screened to identify differentially expressed genes (DEGs) and their associated signal pathway, expression regulation, and metabolic pathways. These findings could help determine an effective target for future monkeypox disease treatment.
About the Study
To evaluate the impact of monkeypox infection on human cells at the transcript level, molecular sequencing datasets, namely GSE36854 and GSE11234, were obtained from the Gene Expression Omnibus (GEO) database. GSE36854 dataset contained eight samples of Vaccinia virus strain IHD-W, Vaccinia virus strain Brighton Red, Monkeypox virus strain MSF infected Hela cells, and blank control.
GSE11234 dataset was based on GPL6763 which comprised many types of poxvirus and human genome template information. The monkeypox-infected Hela cell samples were analyzed to observe genomic changes. The molecular sequences were processed and visualized to identify significantly uniquely expressed genes
Study Findings
A total of 84 DEGs, except histone genes, were found, which were used for further studies. Viral interactions rely heavily on early genes to infect host cells, ensuring their survival, replication, and transmission. These genes are also associated with the regulation of host immunity. Therefore, the gene expression status of the monkeypox virus was analyzed, and 26 suspected early genes were detected, which encoded for the ankyrin repeat protein.
Comparing the sequencing data of many monkeypox samples from the 2022 epidemic and the D1L gene documented in 2018 from the UK, several site mutations were observed. These mutations might be responsible for better adaptation in the human host and enhanced human-to-human transmission.
The changes in the internal body due to external stimulation could be studied by analyzing signal pathways. It was observed that DEGs of monkeypox-infected Hela cells were associated with KEGG signaling pathways, such as TNF signaling pathway, IL-17 signaling pathway, NF-kappa B signaling pathway, cytokine-cytokine receptor interaction, C-type lectin receptor signaling pathway, Kaposi sarcoma-associated herpesvirus infection, Th17 cell differentiation, NOD-like receptor signaling pathway, small cell lung cancer, and human T-cell leukemia virus infection. This finding indicates that monkeypox infection triggers immune responses and produces an inflammatory response.
Genetic disease (GD) analysis was conducted to predict the relationship between monkeypox DEGs and different diseases. This analysis revealed the association of monkeypox infection with liver cirrhosis, reperfusion injury, mammary neoplasms, inflammation, hypertensive disease, juvenile arthritis, and brain ischemia. The findings of this study were consistent with previous reports that revealed complications and sequelae of monkeypox. Furthermore, the current study also observed a link between monkeypox infection and the manifestation of schizophrenia and mental depression.
The role of prostaglandin-endoperoxide synthase 2 (PTGS2), also known as cyclooxygenase 2 (COX-2), has not been reported regarding monkeypox infection. However, based on available evidence related to other diseases, it was assumed that the monkeypox virus regulates the pathological process by controlling PTGS2.
The hub genes, such as IFIT1, IFIT2, IER3, ZC3H12A, IL11, EREG, IER2, FST, NFKBIE, and AREG, of monkeypox-infected HELA cells were extracted. Typically, hub genes are associated with various biological processes. The authors identified the key transcription factors that regulate hub genes, i.e., IRF1, GLIS2, SIN3A, FOXJ2, Smad5, ZFX, and ATF1, and miRNAs (e.g., hsa-mir -21-3p, hsa-mir-16-5p, hsa-mir -520c-3p, hsa-mir -1343-3p, hsa-mir-335-5p and hsa-mir -203-3p).
Conclusions
The current study revealed that the monkeypox virus inhibits two anti-viral genes, namely, IFIT1 and IFIT2. In addition, bioinformatic analysis through the CellMiner database indicated that AP-26113 (Brigatinib) and Itraconazole hold promise for monkeypox infection treatment.
*Important Notice
bioRxiv publishes preliminary scientific reports that are not peer-reviewed and, therefore, should not be regarded as conclusive, guide clinical practice/health-related behavior, or treated as established information.









 Add Category
Add Category

