An article published in Critical Reviews in Food Science and Nutrition journal provides an overview of the role of gut microbiota in shaping the host immune response to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2).
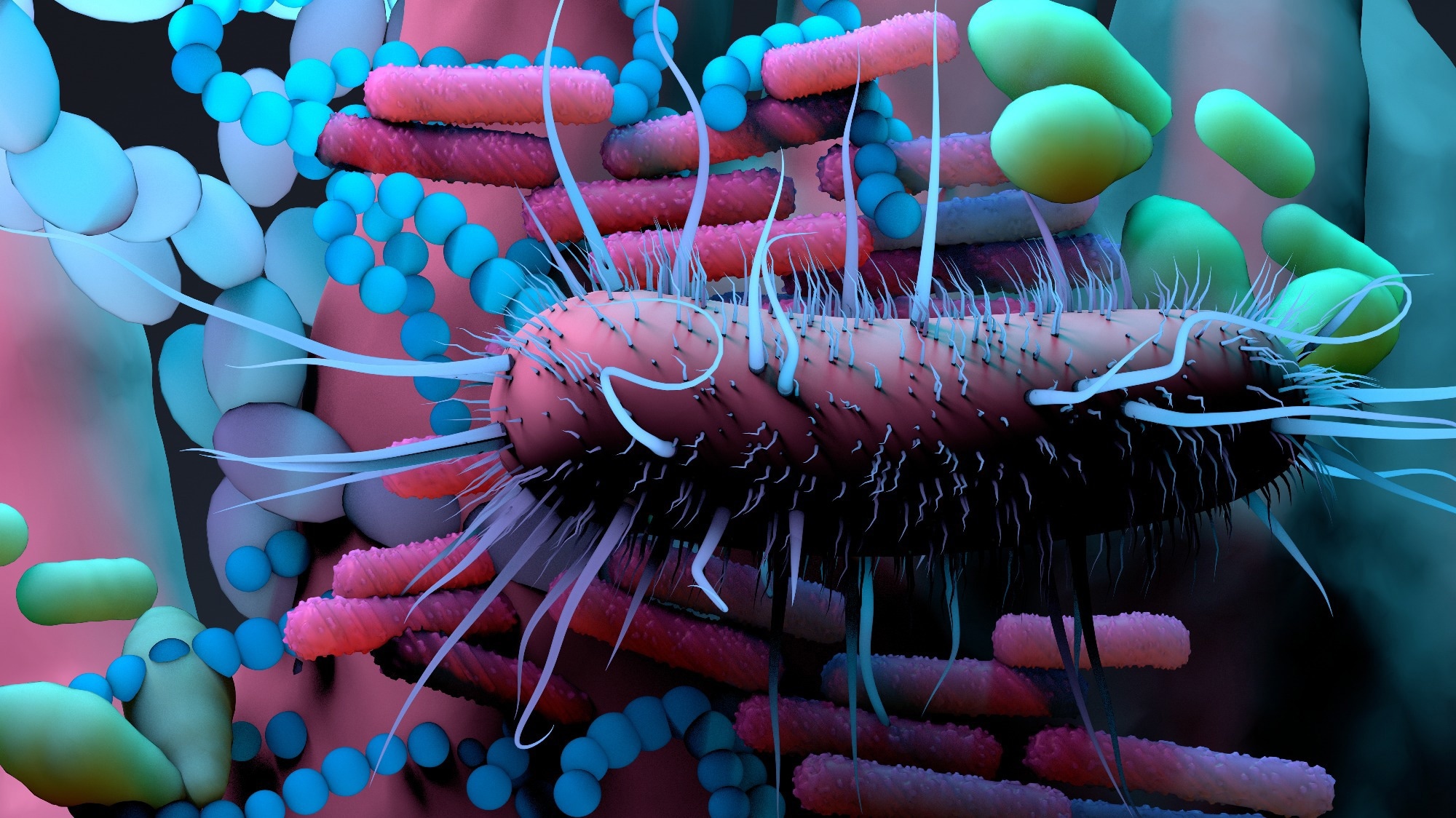 Study: Gut microbiome and anti-viral immunity in COVID-19. Image Credit: Design_Cells / Shutterstock
Study: Gut microbiome and anti-viral immunity in COVID-19. Image Credit: Design_Cells / Shutterstock
Background
SARS-CoV-2, the causative pathogen of the coronavirus disease 2019 (COVID-19) pandemic, is an RNA virus that primarily affects the upper and lower respiratory tract. The virus is also known to potentially target the gastrointestinal (GI) tract and impair the composition and diversity of gut microbiota.
The gut microbiota is a collection of microbes that naturally live in the GI tract. The GI tract contains trillions of microbes that interact with one another to regulate various physiological processes, including the immune system. Alteration in gut microbiota composition and diversity is called dysbiosis, which impairs immune response and inflammation.
Gut microbiota and COVID-19
GI symptoms, including nausea, vomiting, and diarrhea, have been observed in 60% of COVID-19 patients. An impaired gut microbiota has been observed in COVID-19 patients, irrespective of the presence of GI symptoms. Importantly, it has been observed that dysbiosis persists for up to 6 months after the clinical clearance of SARS-CoV-2 from the respiratory tract.
Gut microbiota alterations commonly observed in COVID-19 patients include reduced commensal bacterial populations with immunomodulatory functions that help maintain the integrity of GI barrier and immune homeostasis.
A significant proportion of COVID-19 patients develop long-term symptoms, which is medically termed as long-COVID. Studies have shown that people with long-COVID have reduced commensal bacterial population and altered overall gut microbiota. In addition, the reduced bacterial population correlates with increased serum concentration of proinflammatory mediators in these patients.
A reduction in commensal bacterial population is accompanied by enrichment of pathogenic bacterial population and reduction of gut microbiota diversity. Studies have suggested that these changes in gut microbiota composition and diversity might be associated with increased gut permeability, microbial translocation, hyperinflammation, and poor COVID-19 prognosis.
Besides bacterial population, SARS-CoV-2 infection is known to alter the gut fungal population. An enrichment in opportunistic fungal pathogens has been observed in COVID-19 patients. Pathogens such as these are associated with pneumonia and respiratory symptoms and affect the assembly of gut bacteria.
Gut microbiome and SARS-CoV-2 host cell entry
The spike glycoprotein of SARS-CoV-2 interacts with host cell membrane receptor angiotensin-converting enzyme 2 (ACE2) to initiate the viral entry process. Besides respiratory epithelial cells, ACE2 is expressed at a high level in the stomach, ileum, and colon, highlighting the possibility of direct viral entry into the GI tract.
The abundance of certain bacterial species that downregulate ACE2 expression are known to correlate negatively with COVID-19 severity. Patients with diabetes or obesity exhibit a low abundance of these bacteria and are at the highest risk of COVID-19-related mortality.
Gut microbiome and immune response to SARS-CoV-2 infection
The gut microbiota is known to stimulate host antiviral immune response by modulating type 1 interferon signaling. In severe COVID-19 patients, an impaired interferon response and a suppressed adaptive immune response are known to cause lung damage. SARS-CoV-2-induced alteration in gut microbiota might be associated with these pathologies.
Inflammasome, a cytosolic multiprotein complex, is known to associate with COVID-19 pathogenesis. Recent evidence has suggested that inflammasomes induce the release of neutrophil extracellular traps by neutrophils in severe COVID-19 patients, which in turn is associated with impaired lung function.
An altered gut microbiota might contribute to COVID-19 pathogenesis by triggering inflammasome activation. For example, in COVID-19 patients with cardiac disorders, increased activation of inflammasomes and elevated markers of a leaky gut, such as lipopolysaccharide-binding protein, have been observed.
The gut microbiota is vital for the regulation of the adaptive immune system. For example, in response to viral infection, the gut microbiota induces activation of B cells and T cells, thus participating in antibody production and virus-specific memory immune cell production.
The administration of specific commensal bacteria has been found to increase neutralizing antibody levels in the blood in response to viral vaccination. Similar effects have been observed in COVID-19 patients.
Gut–lung immune axis
The gut microbiota plays an essential role in regulating lung health. Immune cells are migrated from the gut to the respiratory tract to destroy invading pathogens. This is called the gut–lung immune axis.
Alteration in gut microbiota composition increases the risk of respiratory diseases, such as asthma. In COVID-19 patients, opportunistic upper respiratory tract bacteria have been identified in the gut microbiota. Similarly, an imbalance in lung microbiota has been observed in COVID-19 patients with dysbiosis. These observations highlight the occurrence of bidirectional translocation of microbes between the gut and lung.
Modulation of gut microbiota as a therapeutic intervention for COVID-19
Given the significant association between dysbiosis and anti-SARS-CoV-2 immune response, modulation of gut microbiota has been considered a potential therapeutic intervention for COVID-19.
Transplantation of fecal microbiota, which represents the whole gut microbiota, from a healthy donor into the GI tract of a recipient is considered a potential strategy to treat bacterial infection. This strategy is currently under clinical investigation in COVID-19 patients.
Dietary prebiotics are non-digestible fibers used to increase the proportion of commensal bacteria and reduce the proportion of pathogenic bacteria. There is evidence suggesting the health benefits of prebiotics in COVID-19 patients.
Probiotics are live organisms with immunomodulatory effects. In addition, peptides produced by probiotics have shown ACE2 inhibitory effects. Thus, probiotics are considered a potential adjuvant strategy in treating COVID-19 patients.








 Add Category
Add Category

